What is it?
The condition is thought to result from abnormal brain perfusion due to endothelial dysfunction, which causes a failure of autoregulation and leads to cerebral vasogenic edema. It is not yet completely understood, though.
It is also known as posterior reversible encephalopathy syndrome (PRES), which is somewhat of a misnomer because it can involve areas beyond the “posterior” cerebral regions, and it can sometimes cause progressive and permanent injury, thus not being reversible.
Other nomenclatures for this condition include acute hypertensive encephalopathy and reversible posterior leukoencephalopathy syndrome (RPLS).
It’s named because it’s often reversible once BP normalizes (or precipitating factors are removed). Involvement of the brainstem and deep white matter is less reversible than cortical/subcortical involvement.
When to consider this diagnosis?
The classic presentation includes a patient experiencing headache, seizures, altered consciousness, and visual symptoms. Caution: Hypertension does not necessarily need to be present!
Associated conditions
However, various conditions are associated with PRES, and some happen to involve hypertension. The list includes:
- Systemic hypertension
- Preeclampsia, eclampsia
- Chemotherapy agents
- Cyclosporin
- Cisplatin
- Thrombotic microangiopathies
- Disseminated intravascular coagulation (DIC)
- Thrombotic thrombocytopenic purpura (TTP)
- Hemolytic uremic syndrome (HUS)
- Malignant hypertension
- Uremic encephalopathies
- Severe infection
- Septic shock
Patients in Clinical Vignettes
- Pregnant female with
- systemic hypertension
- preeclampsia/eclampsia
- Adult on chemotherapy
- Child with kidney disease or transplantation
What are imaging findings?
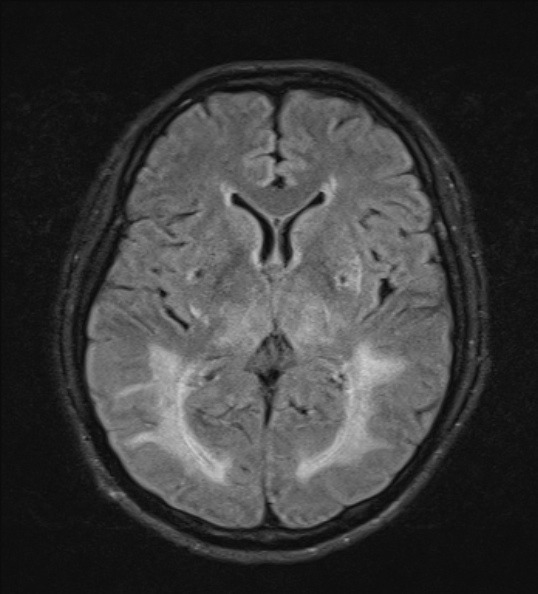
Vasogenic edema

The classic finding is patchy parietooccipital cortical/subcortical edema (90%). This may be subtle or not visualized on CT, thus if clinically suspected, an MRI may be performed to confirm the diagnosis.
Other area that can show edema change including
- Superior frontal lobes (70%)
- Temporal lobes (60%)
- Cerebellum (50%)
- Basal ganglia (30%)
- Midbrain (<20%)
- Pons, medulla, splenium of corpus callosum (<10%)
- Watershed zones
Which areas of involvement are considered atypical? It depends on who you ask, as expert opinions vary.
On MRI, edema appears as T2/FLAIR hyperintensities with no restriction on diffusion-weighted imaging (DWI), indicating vasogenic rather than cytotoxic edema.
The size, extent, and pattern of edema are highly variable; however, it is classically characterized by asymmetric bilateral patchy involvements. Sometimes, lesions become confluent.
It rarely presents with exclusive brainstem involvement—other differential diagnoses should be considered first.
Contrast enhancement
As expected in pathology with vasogenic edema, which results from a breakdown of the blood-brain barrier and vascular leakage, the lesions should demonstrate contrast enhancement. This is evident with variable gadolinium enhancement pattern on MRI imaging, but not with iodine contrast on CT.
On contrast-enhanced CT (CECT), enhancement is usually not observed. If present, it will be mild and may appear as patchy or punctate enhancement.
Hemorrhage
Petechial hemorrhage is a less common finding which can be seen on NECT as punctate hyperdensity involving cortical/subcortical or basal ganglia.
On MRI, three patterns of hemorrhage can be seen.
- Focal parenchymal hemorrhage
- Microhemorrhages
- Convexity subarachnoid hemorrhage (SAH)
The T2* GRE sequence is particularly helpful as it can easily visualize blood products as blooming artifacts.
What conditions can present with similar imaging findings?
Hypoglycemia
This condition can also cause severe parietooccipital edema, so clinical history is, as always, of utmost importance.
Reversible cerebral vasoconstriction syndrome
Many findings similar to PRES but typically limit to solitary sulcus or few adjacent sulci.
Status epilepticus
It may cause transient gyral edema and enhancement, but this is mostly unilateral (PRES is usually bilateral).
Leave a Reply