Scenario
Your patient complains about a soft, non-tender, palpable, movable lump on her back. She is in her thirty and further told you that the lump is slow growing over last 2 years. After examining the lesion, you arrive at lipoma as your most likely diagnosis. You send your patient for an ultrasound exam, and it is “confirmed” to be a fat-containing lesion. Feeling reassured that it is just a lipoma, you provide your patient with reassurance and advise that no further management is needed. Case closed, or is it?
When we encounter a fat-containing lesion in soft tissue, for example, in subcutaneous tissue, we are most likely to think of it as a lipoma. While soft tissue lipomas are benign and the most commonly encountered tumors in clinical practice, various less common pathologies, including some malignant tumors, may mimic this condition, both clinically and at imaging. Therefore, it is crucial for physicians to thoroughly evaluate and differentiate it from such conditions to prevent misdiagnosis and inadequate resection.
Abbreviations
WDLPS = well-differentiated liposarcoma, ALT = Atypical lipomatous tumor, DDLPS = dedifferentiated liposarcoma
Soft tissue lipoma
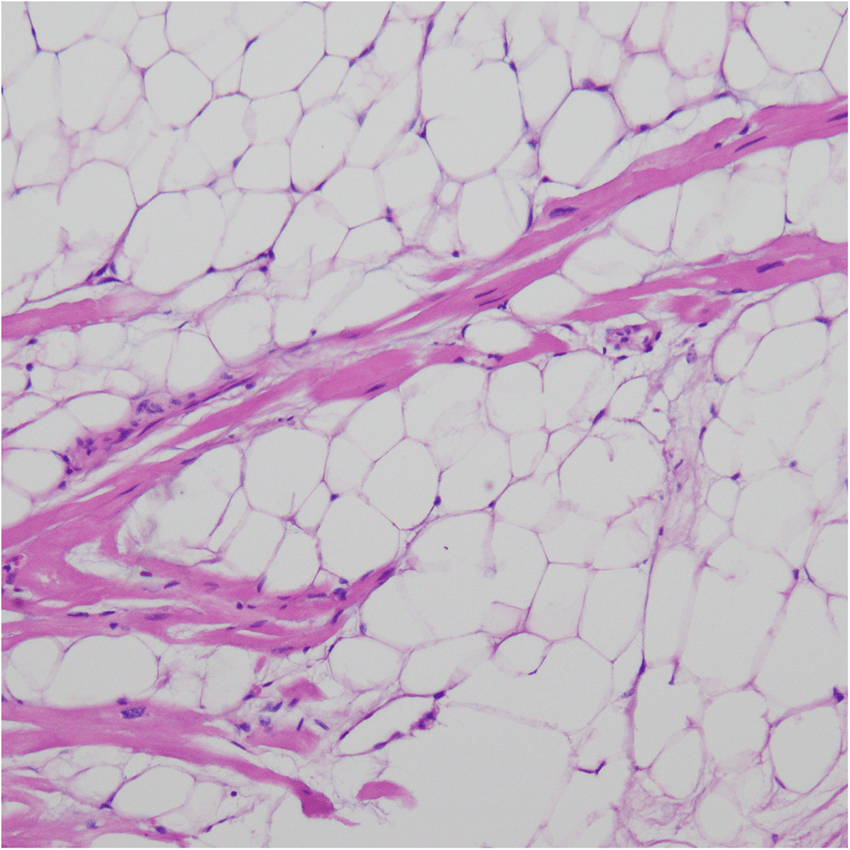
In addition to being the most common soft tissue tumor, lipomas are also the most common benign soft tissue tumors. Classically, a lipoma is homogenously composed of mature adipocytes. Approximately 80% of lipomas are found in subcutaneous tissues, where they sometimes are difficult to distinguish from adjacent subcutaneous fat. Other common locations include intermuscular and intramuscular tissues.
Manifestation and some unusual characteristics
A lipoma typically presents as a painless soft-tissue mass, but occasionally, due to nerve compression, it can be painful.
It is usually solitary, but in 5%-15% of cases, multiple lipomas may occur.
While subcutaneous lipomas are usually encapsulated. Intramuscular lipomas are prone to infiltrate muscle compartments (in 83% of cases), and may sometimes extend into tendons and fascia, exhibiting extramuscular extension.
If a lipoma is involving synovial lining, the patient will come with different chief complaint, mostly gradual painless unilateral knee joint swelling. The condition is called “lipoma arborescens” and not really present with palpable lump as in this scenario.
Imaging
Ultrasound
- Well-defined lesion
- Echogenicity and echotexture similar to subcutaneous fat
MRI
- Sharply bordered lesion
- Signal intensity matching subcutaneous fat (high signal intensity in both T1WI, T2WI)
- Suppresses with fat saturation
- Markers can be placed near the borders of the lesion to aid in differentiating it from the surrounding fat.
Non-fat component in lipomas
Lipomas may contain regions of non-adipose tissue which may cause confusion with other tumors at imaging.
Differential diagnosis of non-fat components includes:
- Entrapped muscle fibers in intramuscular lipomas → sometimes difficult to distinguish a deep lipoma with WDLPS/ALT.
- Calcifications and/or ossifications → dystrophic calcification (usually resulting from previous trauma and hemorrhage)
- Fat necrosis → can demonstrate any findings and is difficult of differentiate from liposarcoma
- Chondroid matrix: may exhibit characteristic calcification = chondroid lipoma
Chondroid lipoma
A rare, benign, slow-growing tumor usually seen in the 3rd to 4th decades of life, more common in women.
In MRI, chondroid regions may resemble myxoid liposarcoma or extraskeletal myxoid chondrosarcoma.
In PET/CT, there is hypermetabolic activity.
Effectively, malignancy cannot be excluded by imaging alone, and a tissue diagnosis is usually necessary.
Spindle cell lipoma (SCL)
Spindle cell lipoma or pleomorphic lipoma histologically presents with a variable proportion of mature adipocytes, spindle cells without atypia, and myxoid stroma. Similar to chondroid lipoma, it is challenging to exclude malignancy through imaging alone.
Both tumors may benefit from preoperative image-guided biopsy to avoid more aggressive surgery for liposarcoma.
Is it really a lipoma?
Since lipoma is the most common soft tissue tumor. It is generally correct diagnosis if you tell your patient that their soft tissue fat-containing lesion is a lipoma. However, you should also consider other possibilities including:
Angiolipoma
Another benign, fat-containing tumor composed of mature adipose cells and small (capillary sized) blood vessels.
Demographic: 2nd-3rd decades of life
Manifestation: multiple, small (<2 cm), subcutaneous, tender nodules, in the forearm, trunk or upper arm.
Treatment: Resection
Prognosis: No report of recurrence or malignant transformation
Hibernoma
A rare, benign, slow-growing soft-tissue tumor with prominent vascularity composed of brown fat arises in regions where vestiges of fetal brown fat persist. Histologically, there is an admixture of immature adipocytes, brown fat cells, and mature adipocytes.
It is usually painless, and the overlying skin may feel warm due to increased mitochondrial activity of the brown fat, causing very high avidity in PET/CT scans.
There are four histologic variants of hibernoma. A lipoma-like variant, when found in retroperitoneal region, can be difficult to distinguish with WDLPS. Myxoid variant can mimic myxoid liposarcoma. Spindle cell variant can resemble spindle cell lipoma.
Lipoblastoma
Avoid diagnosing lipoma in infants or toddlers, as lipomas typically occur in the 5th-6th decade of life, while this tumor mostly presents in patients under 3 years of age. What may be reassuring is that liposarcoma is also extremely rare in children aged less than 5 years.
Lipoblastoma accounts for 30% of adipocytic tumors in children. It often presents as a rapidly enlarging, painless mass with occasional compressive symptoms such as Horner syndrome, respiratory compromise, spinal cord compression, or hemiparesis.
In addition to normal fat composed of mature adipocytes, the lesion contains non-fat components including tissues composed of lipoblasts (immature adipocytes), myxocollagenous stromal tissue (myxoid), intratumoral infarction, and mucoid/cystic degeneration.
In MRI, the lesion will show a heterogeneous texture with T1-hypointense + T2-hyperintense areas, representing its non-fat components. High signal intensity areas in T2FS images are highly suggestive of the myxoid component and are never found in lipomas.
Both lipoblastoma and hibernoma are composed of immature fat, which is typically slightly hypointense relative to subcutaneous (mature) fat on T1-weighted images and may not be suppressed in fat suppression sequences.
Lipoblastoma may later evolve into a mature lipoma or invade surrounding tissue (lipoblastomatosis). However, it has no metastatic potential, so it is considered benign.
Treatment
- Wide excision
- Given the potential for spontaneous regression and the lack of malignant transformation, it is worth considering avoiding mutilating surgery.
Prognosis:
- Lipoblastoma: recurrence is rare.
- Lipoblastomatosis: 10-25% recurrence rate
Differential diagnosis:
- Teratoma (if containing calcifications)
- Lipoma
- Well-differentiated liposarcoma (WLDS)
No distinguishing imaging’s features but can reliable excluded by age. - Dermoid cyst
So, there are also fat-containing lesions that are not really lipomas but still considered benign. However, from this point onward, we will discuss more aggressive types of tumors.
Atypical lipomatous tumor (ALT)
ALT is a low-grade malignancy composed predominantly of fat, also termed well-differentiated liposarcoma (WDLPS). It is locally aggressive but non-metastasizing. It is the most common type of liposarcoma, most frequently located in the deep tissues of the extremities; the thigh is most common. Superficial soft tissue involvement is rare.
ALT has a peak incidence in 50-80 years old with no sex predilection. It is painless, slow-growing and can attain a very large size, usually > 10 cm.
Imaging
MRI is a useful tool for differentiating between lipomas and other malignant lipomatous tumors. Non-fat components are suggestive of atypical lipomatous tumor (well-differentiated liposarcoma).
Non-fat components
- Nodules
- Thickened septa (> 2mm)
- Areas of irregular or nodular enhancement
Histological subtype
- Adipocytic (lipoma-like)
- Sclerosing → unfavorable prognostic factor for local recurrence, most often occurs in the peritoneum
- Inflammatory → rarest
Treatment = wide excision ± RT
Recurrence rates
The median time to local recurrence is 48 months from the date of surgery.
- Extremities, trunk, and abdominal walls: 23-43%
- Retroperitoneum, mediastinum and paratesticular: 90-100%
Because of marked differences in prognosis, many authors use the term ‘ALT’ for more favorable tumors involving extremities, trunk, and abdominal walls, while using ‘WDLS’ for more ominous tumors involving the retroperitoneum and paratesticular.
Differential diagnosis
- Myolipoma (lipoleiomyoma) is a rare benign neoplasm composed of mature adipose tissue and mature smooth muscle cells. It is most commonly seen in adult women and arises within the abdominal cavity, retroperitoneum, or inguinal regions.
Liposarcoma
Liposarcoma ranks as the second most common soft tissue malignancy in adults, following undifferentiated pleomorphic sarcoma. Typically afflicting individuals over 60 years old, the majority of cases (75%) arise in the lower extremities. Subtypes include ALT/WDLPS, dedifferentiated liposarcoma (DDLPS), myxoid liposarcoma, and pleomorphic liposarcoma.
The appearance of liposarcoma varies in MRI, making it challenging to determine solely through imaging. However, MRI plays a crucial role in surgical planning and guiding tissue biopsy of the non-fat component.
This malignancy can metastasize to soft tissues, lungs, liver, and bones, necessitating imaging evaluations for both primary tumor and distant metastasis in treatment planning.
Treatment = wide excision ± radiation therapy ± chemotherapy.
Prognosis: worsen with a greater proportion of round cell components in histology.
Dedifferentiated liposarcoma (DDLPS)
Dedifferentiated liposarcoma (DDLPS) is the most prevalent type of liposarcoma, arising from well-differentiated liposarcoma (WDLPS) in 17% of cases and atypical lipomatous tumors (ALT) in 6%. The risk of DDLPS increases with each recurrence. Typically, DDLPS presents as a sizable mass at diagnosis, demonstrating local invasion into adjacent structures. Awareness of this condition in ALT/WDLPS cases is crucial for detecting early complications beyond recurrence.
Myxoid liposarcoma
Myxoid liposarcoma, the second most common type of liposarcoma, is considered to be part of a histological continuum with round cell liposarcoma. Pure myxoid liposarcoma is categorized as a low-grade sarcoma, with a metastasis risk of less than 10%. Conversely, myxoid liposarcoma with more than 5% round cell component is deemed a high-grade sarcoma with a worse prognosis.
Predominantly occurring in deep soft tissues of the extremities, the thigh serves as the most common location for myxoid liposarcoma. In comparison to other soft-tissue sarcomas, myxoid liposarcoma exhibits a higher incidence of extra-pulmonary metastasis to soft tissues and bones.
On MRI, pure myxoid liposarcoma presents as a encapsulated mass with a characteristic low T1 and markedly high T2 signal. The non-fatty non-myxoid (round cell) component in high-grade myxoid liposarcoma displays intermediate T2 signal and variable enhancement. Higher-grade myxoid liposarcoma is commonly associated with features like vascular and bone invasion, circumferential vascular encasement, absence of a pseudo-capsule, and the presence of tumor necrosis.
Differential diagnosis
- Intramuscular myxoma
- Extraskeletal myxoid chondrosarcoma
- Complicated cystic lesion (hemorrhage)
Pleomorphic liposarcoma
For the sake of completeness, we mentioned pleomorphic liposarcoma, although it is not a fat-containing lesion. It is, in fact, the least prevalent type of liposarcoma. Pleomorphic liposarcoma typically does not exhibit any fat component. Histologically, it is composed of cells with marked pleomorphism, a paucity of lipid, and a significant amount of mucin. Imaging usually reveals a large (>10 cm) heterogeneous myxoid mass with areas of necrosis and/or hemorrhage. However, these features are not specific and cannot be reliably differentiated from other high-grade soft tissue sarcomas.
Afterthought
Two years later, you encounter your patient again, this time with gastrointestinal symptoms as her chief complaints. During the clinical history discussion, she discloses that since your first visit, the lump on her back had grown larger, causing discomfort when lying down. Subsequently, she chose to have it excised at another hospital, and the histology results confirmed it was indeed a lipoma. While uncommon for a 30-year-old, this case serves as a reminder that nothing in medicine is absolute. Moreover, lipoma remains the most common fat-containing lesion in adults.
In general, the diagnosis of superficial small lipomas can be reliably confirmed with ultrasound examination, helping to alleviate excessive worry and prevent ineffective use of resources. MRI may be considered when features associated with higher aggressiveness, such as larger size (>10 cm) or deeper locations (beneath peripheral deep fascia), are suspected.
In cases where further investigation is needed, it’s essential to be aware that 8% of superficial lipomas may show non-fat components, potentially causing false-positive imaging interpretations. Conversely, if a tissue biopsy is performed, false-negative results can occur if the sample only contains mature adipocytes. We hope this article will assist you in appropriately managing “lipoma.”
Leave a Reply